Adenosine: Story, Science, and Significance
Historical Development
Adenosine burst onto the scientific scene in the late 1920s, born out of efforts to dig deeper into the building blocks of life. For nearly a century, scientists have unraveled layer after layer of the molecule’s role within human biology. Progress came slowly at first, with papers trickling in about its place in energy transfer and signal regulation. By the 1950s, researchers recognized adenosine’s central role in ATP-driven processes, which power nearly every action in the human body, from muscle contraction to nerve signaling. In the decades since, teams across the globe have cataloged its impact, exploring its influence on the heart, brain, and immune responses. No university lab or pharmaceutical bench has ever looked at adenosine as just another compound on the shelf. Its status as a molecular messenger and metabolic workhorse turned it into a focus point in research circles, and now forms the backbone of medical treatments, basic research, and drug development.
Product Overview
Adenosine comes in white, crystalline powder or as a prepared sterile solution, ready for research or medical use. Laboratories rely on its stable, highly soluble format for everything from cell signaling studies to pharmacological evaluations. Physicians turn to its injectable form, which is short-acting and reliable. Regulatory bodies demand tight control of the production process, tracking everything from raw materials down to packaging labels, so the product always matches the strict requirements set for clinical and experimental purposes. Each batch typically includes a Certificate of Analysis, guaranteeing compliance with pharmacopeial standards.
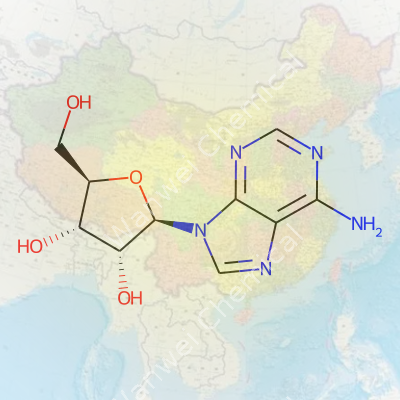
Physical & Chemical Properties
This molecule boasts the formula C10H13N5O4, a relative heavyweight among nucleosides. Its molecular weight sits at about 267.24 g/mol. Its melting point hovers near 235°C, which is high enough to signal solid thermal stability. Adenosine’s solubility in water, around 80 mg/ml, makes it ideal as a research reagent and injectable drug. The molecular structure — a ribofuranose sugar joined to an adenine base — holds the secret to its biological activity. In biological systems, this means rapid recognition and tight regulation. In a vial, it means technicians and researchers don’t wait long for it to dissolve or activate.
Technical Specifications & Labeling
Each vial or bottle of adenosine comes stamped with lot number, manufacture date, purity (often >99%), and clear storage instructions. Clinical grade adenosine also lists sterility and endotoxin thresholds. Some vials feature single-use recommendations due to the molecule’s high reactivity in solution. Packaging often includes temperature indicators, because time on the shelf or in a transport truck stresses stability. Actual labeling spells out contraindications, for example warning about using it in patients with certain heart conditions. Regulatory agencies, including the FDA, require manufacturers to produce detailed product inserts explaining potential risks, usage protocols, and likely side effects.
Preparation Method
Laboratories manufacture adenosine through either extraction from yeast and other sources or total synthesis. Chemical synthesis typically starts with protected ribose derivatives, which undergo reaction with adenine in carefully controlled conditions. Some producers stick with fermentation from natural sources, counting on established purification steps like chromatography to yield a highly pure end product. Some manufacturers go with enzymatic methods, harnessing the specificity of nucleoside phosphorylases for large-scale or specialty production. Each approach has its fans and detractors, with decisions usually hinging on cost, yield, and purity needed for the end application.
Chemical Reactions & Modifications
In the hands of a skilled chemist, adenosine serves as a backbone for preparing adenosine phosphates (AMP, ADP, ATP) and analogs with clinical or experimental value. Chemical modification at various positions, such as the 2′ or N6 group, creates compounds with subtle shifts in biological behavior. These tweaks enable selective inhibition or activation of target enzymes and receptors. In pharmaceutical circles, slight modifications produce molecules powerful enough to trigger heart rhythm resets or dial down immune reactions. Research pushes these synthetic skills to their limits, generating new ligands for adenosine receptors, paving the way to novel therapeutics.
Synonyms & Product Names
Adenosine hides behind plenty of names and codes. You see “Adenocard” and “Adenoscan” in hospitals, and simple “adenosine” in both pharmaceutical supply and research shops. Academic researchers spot it as “9-β-D-Ribofuranosyladenine” on chemical inventories. Other variants and analogs like 2-chloroadenosine or N6-cyclopentyladenosine fill out the chemical family, each gaining attention for their specific laboratory or clinical uses.
Safety & Operational Standards
Handling adenosine safely means strict attention to detail. Lab workers don goggles and gloves when working with powders or concentrated solutions. Medical staff monitor patients closely during administration, because it can trigger dramatic effects on heart rhythm. Material Safety Data Sheets warn users about potential routes of exposure and necessary protective equipment. Hospitals that use the molecule keep crash carts and resuscitation gear nearby. Disposal of unused or expired product follows hazardous pharmaceutical guidelines, and records stick around for years in case regulators or auditors swing by.
Application Area
Hospitals use adenosine as a fast-acting antiarrhythmic. Doctors inject it to break attacks of supraventricular tachycardia, counting on its ability to put the brakes on runaway electrical signals in the heart. Radiologists count on adenosine to induce stress during myocardial perfusion imaging. Outside medicine, molecular biology labs use it as a research tool, testing the behavior of adenosine receptors and charting cellular metabolism. Some vaccine and drug developers build adenosine analogs to manipulate immune response or fight infections. Its influence crosses into neuroscience and immunology, where it helps map networks of signaling and cell differentiation.
Research & Development
Major R&D investments flow into finding new uses for adenosine and its analogs. Pharmaceutical companies race to design more selective receptor agonists or antagonists, hoping to harness its tissue-specific effects. Chemists develop stable derivatives, aiming for longer half-life or improved oral delivery. Teams study the interplay of adenosine with cancer biology, immune suppression, and central nervous system disorders. Each project leans heavily on collaboration — chemists, pharmacologists, and clinicians sharing data from bench to bedside.
Toxicity Research
Careful studies chart the line between therapeutic and toxic doses. In the clinic, too much adenosine produces flushing, chest discomfort, hypotension, or even heart block. For years, researchers have monitored patient outcomes after bolus injections, tracking adverse events and recovery rates. Animal studies catalog acute and chronic effects, noting impacts on respiration, metabolism, and the central nervous system. Scientists raise questions about the impact of long-term exposure to adenosine analogs, especially with the growing interest in receptor-targeting drugs for chronic conditions. Regulators stay on their toes and keep re-examining dose thresholds, warning labels, and injection protocols.
Future Prospects
Interest keeps growing for adenosine-based therapeutics in autoimmune disorders, cancer immunotherapy, and pain management. Research into modified analogs and drug delivery systems expects to yield treatment options with less severe side effects and longer duration. Personalized medicine teams are looking for ways to match adenosine receptor subtype profiles with specific patient groups. Its double-duty as a metabolic regulator and signaling molecule means it won’t lose its place in physiology textbooks anytime soon. More collaborations are coming between industry, academic groups, and regulatory agencies to unlock its full clinical potential while ensuring safety and accessibility across new disease areas.
A Quick Dive Into Adenosine’s Role in Healthcare
Walk into an emergency room and odds are somebody has seen adenosine at work. Doctors rely on it during high-pressure moments, and for good reason. It’s a medication that’s saved lives by jarring the heart back into the right beat. In the middle of a rapid heart rhythm, specifically a type known as supraventricular tachycardia, adenosine helps reset the heart’s rhythm almost like flipping a circuit breaker.
How Adenosine Affects the Heart
Adenosine isn’t some foreign chemical cooked up in a lab just for hospitals; the body actually makes its own. Inside every cell, it handles energy transfer—think ATP, the molecule we hear athletes talk about. In medicine, the injectable version grabs doctors’ attention because it slows down electrical signals in the heart. With one quick IV push, the medication blocks those signals for a brief moment, letting the heart’s natural pacemaker reset itself. My own years in healthcare taught me that seeing someone’s heart rhythm shift from chaos to calm on a monitor impresses everyone in the room. It’s an instant reminder that science has teeth, and the right tools can make the difference in seconds.
Safety and Side Effects—What Patients Experience
Giving adenosine isn’t like taking painkillers for a headache. The effects hit fast—patients often notice a hot flush, chest pressure, or a sense their heart skipped a beat. Most feel strange for less than a minute. These odd feelings almost always fade once the heart resumes its natural rhythm. There are risks, like with any tool in medicine. Those with asthma have to watch out. Adenosine can trigger wheezing, so nurses and doctors usually check a patient’s history before pushing the drug.
Why Doctors Trust Adenosine
This trusted medication earned its place partly because it’s quick and the effects vanish fast. In the middle of an emergency—say, a teenager with a racing heart from a dance competition—doctors need something reliable. Since adenosine doesn’t linger in the bloodstream, if it doesn’t work, they can move on to the next step without long delays or worry about buildup.
Adenosine can help clarify what’s actually going on. I’ve seen situations where a strange EKG reading leaves everyone scratching their heads. A short dose of adenosine unmasks the true heart rhythm, which can mean the difference between a quick discharge and a bigger cardiac workup. It’s these small, clear outcomes that build trust in the drug.
Looking Forward
Access to adenosine means emergency teams have a fighting chance in the most frantic situations. Training more staff to recognize the signs of dangerous heart rhythms and act quickly could mean more people benefit from this reliable tool. Hospitals sometimes face shortages; keeping supply chains strong can prevent unnecessary risks for patients. Talking about adenosine brings home how important it is for both ordinary folks and professionals to know what lifesaving treatments exist and how they work in real life. The science behind adenosine isn't distant or abstract—it's part of real emergencies every day across the world.
A Molecule with Real Impact
Adenosine doesn’t get the spotlight like some other molecules, but its job in the body matters more than most people realize. Every cell relies on it, especially as energy ebbs and flows through muscles and the brain. Most folks only think about adenosine when they reach for a cup of coffee, hoping for a jolt of energy. The truth runs much deeper than caffeine’s quick fix.
The Energy Connection
I spent years pulling late nights, staring at screens, trying to power through. Fatigue sneaks up despite best intentions. That heavy, slow feeling? Adenosine builds up in your brain as you go about your day, tying directly to how tired you feel. It’s not just a background process—the more active you are, the more adenosine stacks up. Your brain reads this as a cue to rest.
Caffeine owes its punch to blocking adenosine receptors. Instead of fatigue signals, your brain grants a temporary pass and you feel more alert. This trick doesn’t erase your body’s real need for rest—eventually, adenosine catches up, and that energy debt returns double. What stood out in my own experience: no drink or hack really replaces proper sleep. Studies have shown that people who habitually rely on caffeine actually accumulate more sleep debt over time, with attention lapses becoming more likely as adenosine does its work in the background.
Heart, Blood, and Beyond
Adenosine plays a hand in more than just sleepy afternoons. The heart depends on it to slow things down when they get too hectic. Anyone who’s watched their pulse race after a shock or a run knows that the body doesn’t always control its pace perfectly. When rhythms go haywire, doctors even use a quick shot of adenosine to snap the heart back to a normal beat.
This same molecule helps blood vessels widen, which means better flow and more oxygen delivered where it’s needed—whether that’s thinking through a tough morning or sprinting across a finish line. Researchers point to these effects as protective, keeping tissues healthier under stress. People with cardiovascular conditions sometimes struggle because their adenosine response isn’t working right, highlighting just how essential this simple molecule turns out to be.
Potential Solutions: Rethinking Sleep, Stress, and Stimulants
No shortcut really works in the long haul when it comes to managing adenosine’s effects. Better rest restores balance. The American Academy of Sleep Medicine recommends 7-9 hours per night for most adults; ignoring this stretches your body thin and makes adenosine pile up faster. From my own misadventures with sleep deprivation, resetting a tired brain means putting the phone away and setting up consistent routines instead of chasing that artificial alertness.
Cutting back on caffeine late in the day can help. Since caffeine disrupts adenosine’s message, you may fall asleep later or miss deeper sleep stages. For those working in high-stress jobs, learning to manage stress with breaks and breathing techniques doesn’t just calm nerves—it gives your body room to clear adenosine, so you stop running on empty. Exercise supports this process as well, both by using up stored energy and by improving sleep quality at night.
Building Better Habits for Real Energy
Most adults juggle work, family, and personal plans—meaning fatigue feels like a constant guest. Instead of outsmarting biology, the best strategy means working with what we know about adenosine. Respecting its signals, building routines for real downtime, and thinking twice before masking tiredness with caffeine make a bigger difference than any miracle supplement. The science points us toward rest, not shortcuts, if we want clear thoughts and healthy bodies for the long run.
Feeling Your Heart Race
Adenosine has changed the way doctors treat certain heart conditions, especially something called supraventricular tachycardia (SVT). It works fast and resets the heart’s rhythm like flipping a switch. A jab in the arm, people brace for a boom in their chest. The most common thing folks mention right after an adenosine push is that sudden pounding or flutter in their chest. Some call it a sense of impending doom. It’s scary but usually vanishes in less than a minute.
Racing Against Shortness of Breath
That dose of adenosine brings a breathless feeling to many. You just get this tightness; it’s like you can’t pull in a full breath for a bit. The research behind this shows adenosine can cause the airways to narrow. If you’ve ever had asthma or chronic lung problems, this can turn serious quick. Emergency doctors keep oxygen ready and stare at the clock after every dose for this reason.
Sensing Warmth, Redness, or Pain
Lots of people talk about warmth washing over their face, neck, or upper chest. The body’s blood vessels open up wide as adenosine sweeps through, causing that glowing feeling. It’s harmless and quick, but surprising. I’ve watched patients get flushed, sweat, and ask if they’re having a hot flash. A burning sensation at the injection site happens, too. It fades, but it’s not soon forgotten.
Recognizing Nausea and Headaches
Nausea shows up on the side list, sometimes paired with a pounding headache. Whether lying on a stretcher or sitting upright, a handful of folks turn clammy and green. One study found about 10% feel this after a standard dose. It’s the body’s sudden shift in blood flow that sometimes brings it on. Patients tempted to jump up usually find a few minutes of rest wins the fight against the queasy feeling.
Worst-Case Scenarios
Adenosine isn’t all roses—even if those moments pass quickly for most. People with a history of severe asthma or heart block walk a tightrope. Those rare stories of stopping hearts for longer than expected, or life-threatening breathing trouble, stick with emergency crews. Risk goes up for people with underlying conduction disease or those on certain heart meds. Doctors have to ask the tough questions before giving it, making sure they’re not trading one crisis for a bigger one.
Managing Side Effects in Real World Care
No medicine comes without trade-offs. With adenosine, the payoff sits in its ability to snap the heart out of a bad rhythm, but only in the right hands. Staff keep crash carts nearby, monitor breathing, and coach patients through the wave of strange feelings. Good communication helps lower anxiety, and preparing for side effects keeps bigger problems at bay.
Looking to the Future
Doctors and patients trust adenosine because it works, and because experience has shaped how it is given. Some providers look at alternatives in tough situations—like verapamil—or turn to tailored approaches when adenosine’s risks rise. Listening to the patient, checking their full history, and supporting them through the process make the biggest difference in keeping care safe and effective.
Getting to Know Adenosine
Adenosine shows up often in emergency medicine. Doctors use it to treat certain types of abnormal heart rhythms, especially a rapid heartbeat that starts above the lower chambers of the heart. This isn’t some easy-going home remedy—the drug’s purpose is clear, and so is the risk if misused. While some people might hear “medicine” and assume safety across the board, real-world experience and medical evidence show a different story.
Understanding Adenosine’s Physical Effects
The body naturally produces some adenosine, which plays a role in energy transfer and even sleep regulation. In the emergency room, doctors inject synthetic adenosine into a vein to slow down the electrical signals in the heart for a few moments. In the right situation, the results can be dramatic and lifesaving. Yet every drug with strong effects brings along the potential for strong side effects. Patients can feel chest tightness, shortness of breath, lightheadedness, or a feeling of doom. Most of these effects wear off fast, since adenosine doesn’t stay in the bloodstream long.
Who Faces More Risk?
People with asthma or chronic lung conditions definitely face higher risk if treated with adenosine. The drug can trigger bronchospasm, making breathing harder. For these patients, something as basic as catching a breath can turn into a struggle pretty quickly. Folks with certain heart conditions—like high-degree heart block or sick sinus syndrome—should avoid adenosine except in special cases. With these conditions, adenosine can slow the heart too much, risking a dangerous pause.
Doctors keep a close eye on people who take dipyridamole (a blood thinner), carbamazepine (for seizures), or who receive certain heart medications. Mixing adenosine with these drugs can change how the patient reacts—sometimes making the effects too strong or unpredictable. So, experience shows that even in a hospital’s hustle, a careful check of the patient’s background matters.
Practices that Matter in Real Life
In my experience, the true safety net in giving adenosine doesn’t come only from the drug itself but from having skilled professionals on hand. Nurses and doctors stand ready, with the crash cart never far off. They check—and double check—for any history of asthma, receipts for certain medications, or other red flags. The short, sharp jolt adenosine gives to the heart always happens with at least a little anxiety in the room, especially for patients and families. Every year, healthcare teams update their protocols based on the latest research and safety notices.
How Can We Make Adenosine Use Safer?
Patients should talk through their medication lists and any chronic illnesses with their doctors before any emergency arises. Medical records that travel with the patient—either in electronic form or as an old-fashioned printout—make a difference when seconds count. Hospitals stress teamwork, clear communication, and practice runs for emergency situations. Training helps staff act fast if someone reacts badly to the drug.
Adenosine has a place in modern medicine, but no one should see it as one-size-fits-all. Personal health history always matters. When a life is on the line, skillful hands and up-to-date knowledge mean that the right treatment finds its mark—and keeps avoidable tragedy out of the room.
What Makes Adenosine a Key Player in Emergencies
An encounter with adenosine in a medical setting isn’t likely for most folks. For anyone experiencing supraventricular tachycardia (SVT), doctors often turn to this molecule. In my years volunteering with emergency responders, I’ve watched sterile, chaotic rooms grow quiet as a nurse readies a syringe. The drug does its job right away, so everything tends to slow down for a second — patients and medical staff both notice the shift.
How Doctors Actually Give Adenosine
Adenosine isn’t a pill or a drip. Doctors measure out a tiny dose and deliver it right through a vein, usually using IV push. This method matters. It gives the drug a direct route to the heart. Medical teams often use a “two-syringe” technique: one syringe pushes adenosine, another flushes it immediately with saline, wasted seconds mean less effectiveness. Unlike some medications that work after several minutes, this one produces effects within seconds. Heart monitors show changes almost instantly.
The job of adenosine isn’t to fix the underlying heart problem for good. It interrupts the electrical signal that’s causing the racing heartbeat. Some people describe a short, uncomfortable wave — a feeling of their chest being squeezed, and for a brief moment, a sensation that the heart has stopped, quickly followed by relief as the regular rhythm returns. This feeling, though fleeting, tends to frighten people who aren’t prepared, showing how important it is for medical teams to explain what’s about to happen.
Safety, Challenges, and Training Matter
Adenosine’s power calls for respect and preparation. Giving it outside a hospital demands vision and a well-set protocol. Paramedics train for this because while the drug resets the heart’s rhythm, sometimes it triggers other electrical problems or rarely, a dangerous rhythm. Not every patient qualifies, either. For example, doctors avoid adenosine in people with asthma, severe heart block, or certain irregular rhythms that come from lower chambers of the heart.
Mistakes happen in real life. I’ve seen some medical interns fumble with timing or dosage. That’s why a tight regimen of continuing medical education and simulation drills helps everyone practice before it’s time to step up on the job. Hospitals should keep up-to-date guides on best practices and invest in clear protocols for giving the drug. Emergency departments rely on good teamwork. A nurse calls out “adenosine ready,” another stands ready with the saline, monitoring staff tracks heart rhythm changes, and everyone’s eyes fix on the patient.
The Bigger Picture: Communication and Consent
Because this drug can make people feel like their heart has stopped, honest explanation makes a difference. No one wants to feel blindsided or scared in the middle of a sudden medical crisis. Quick, straight talk works better than medical jargon. “You may feel strange for a few seconds, but we’re right here, and this should help your heart settle down,” has helped many patients I’ve talked to over the years.
Adenosine only sticks around in the body for a few seconds. That fast action makes it both effective for the right use and safe for most people, though a doctor’s assessment always comes first. In the end, the way adenosine is given — by well-prepared hands and communicated clearly — matters as much as the drug itself.