Glucose: The Journey, Science, and Future of an Essential Sugar
Historical Development
Glucose has roots stretching back to the early study of plant chemistry. Back in the 18th century, chemists used rudimentary tools to extract sweet substances from fruits and grains, though they did not know the exact makeup. By the early 19th century, figures like Jean Baptiste Dumas and Michel-Eugène Chevreul managed to pin down the sweet compound from grape juice, later called “grape sugar.” In 1838, Jean-Baptiste Dumas and Jean-Louis Prévost crystallized the identity of glucose, isolating and naming it. Over time, the ability to synthesize glucose from starch and document its stereochemistry paved a path not only for nutrition science but also medicine and industrial production. The 20th century saw deep investigation into the role this monosaccharide played in energy metabolism, diabetes, and even fermentation, each new thread making glucose even more central to food production, pharmaceuticals, and scientific research.
Product Overview
In today’s market, glucose exists both as a pure chemical and a component in many products. Producers offer it as a white crystalline powder, a thick syrup, and in tablet form for pharmaceutical use. Major suppliers convert grain starches—corn and wheat are common in North America and Europe—into glucose using enzymatic hydrolysis. The market splits into medical-grade and food-grade glucose, each batch aligned with specific testing protocols and purity expectations. Looking at a supermarket shelf or pharmacy stand, glucose appears as dextrose, simple syrup, or as a component in oral rehydration solutions, breakfast cereals, baked goods, and infusion bags.
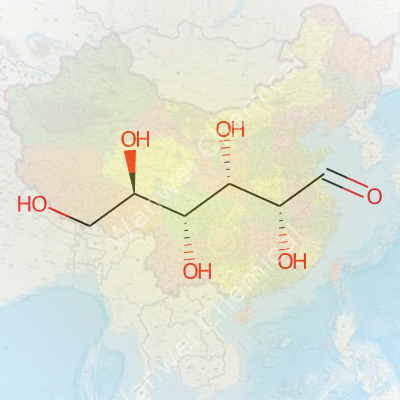
Physical & Chemical Properties
A single glucose molecule contains six carbon atoms, twelve hydrogen atoms, and six oxygen atoms, arranged as C₆H₁₂O₆. The crystalline form melts at around 146°C, showing low solubility in cold alcohol but high solubility in water, which gives it a place in countless recipes and intravenous therapies. Its solutions appear colorless and taste sweet. Glucose swings between a six-membered ring and an open-chain form in aqueous solutions, keeping it versatile in biochemical reactions. Chemically, it holds multiple hydroxyl groups—hydrophilic in nature—making it an excellent reducing sugar. This feature allows it to take part in classic reactions like Fehling’s test and Benedict’s test, where it reduces copper ions, forming colored precipitates. Such tests are still used in lab courses and rural health centers worldwide for diabetes monitoring.
Technical Specifications & Labeling
A look at a glucose product label reveals purity typically above 99%, moisture below 10%, with sulfated ash and heavy metals held to strict limits. Dextrose equivalent (DE) values indicate sweetness and reducing power, a critical figure for food processors. In pharmaceuticals, United States Pharmacopeia (USP) or European Pharmacopeia (Ph. Eur.) standards apply—each batch must pass a battery of checks for endotoxins, microbial load, and optical rotation. Labels on food packaging sometimes confuse consumers; “dextrose monohydrate” and “glucose syrup” mean similar but not identical products, reflecting subtle differences in water content and processing stage. Clearer wording might cut down on consumer confusion, especially among families concerned about diabetes or childhood obesity.
Preparation Method
Industrial glucose production scales up a process first carried out in simple test tubes. Factories soak corn or wheat in water until soft, grind it into a slurry, treat it with amylase enzymes from specialized bacteria or fungi to break starch chains down, and finally introduce glucoamylase to unlock the glucose units. The liquid is filtered, decolorized, and carefully dried, often using vacuum or spray-drying technology, to yield a powder. Pharmaceutical firms take the added precautions of cold filtration and multi-stage purification to ensure pyrogen- and endotoxin-free product. In a typical home kitchen, simple hydrolysis of starch by acid won’t yield pure glucose, underscoring the need for precise control found only in industrial and laboratory settings.
Chemical Reactions & Modifications
Chemists have always gotten creative with glucose’s structure. Oxidizing the aldehyde group on carbon one produces gluconic acid, common in food acidulants and cleaning agents. Full oxidation makes glucaric acid, now tapped for biodegradable polymers. Reducing glucose gives sorbitol, a sugar alcohol present in dental chewing gums and as a humectant in cosmetics. Under high heat, glucose undergoes caramelization—the core of the rich brown flavors in baked bread crusts and confectionery. In Maillard reactions, glucose reacts with amino acids, unlocking flavors and browning foods, though it also raises health concerns over acrylamide formation. Through modern biotechnology, glucose serves as the feedstock for fermentation to produce antibiotics, amino acids, and biodegradable plastics, highlighting its adaptability.
Synonyms & Product Names
Marketing departments and chemists don’t always speak the same language. “Dextrose” often labels the D-isomer of glucose, a dominant form in nature and the human bloodstream. In baking ingredients, “corn sugar” and “grape sugar” refer to specific origins. “Glucose syrup” describes a mixture still containing oligosaccharides and dextrins, with varying sweetness and viscosity. European ingredient lists sometimes show “glukose” or “glucose monohydrate,” all talking about the same base molecule but in slightly different forms. Food companies could probably do better at harmonizing names to cut down on consumer confusion, especially for those tracking sugar intake for metabolic reasons.
Safety & Operational Standards
Each production facility faces regular audits to maintain food and pharmaceutical safety. Operators wear protective gear, control dust, and monitor allergens. The FDA, European Food Safety Authority, and local agencies set standards to block heavy metal or microbial contamination. Labeling covers allergen status, origin, and batch numbers, supporting traceability if a problem appears. Workers learn emergency procedures to handle accidental spills—a rare event due to glucose’s low toxicity, but necessary given powder and syrup handling hazards. Guidelines from bodies like Codex Alimentarius inform allowable uses and levels, updated as new research emerges.
Application Area
More products make room for glucose than many realize. The food sector leans heavily on it for candy, soft drinks, and energy bars. Bakeries use glucose and syrup forms to add sweetness, feed yeast, and build soft crumb structures. In emergency medicine, paramedics reach for glucose gels or tablets to revive a diabetic patient battling hypoglycemia. Hospitals infuse glucose intravenously to hydrate, energize, or support nutrient metabolism. Food technologists rely on its humectant and browning properties in shelf-stable snacks, while industrial chemists use it as a fermentation feedstock to brew everything from citric acid to bioethanol. Recently, sustainable chemical projects started from glucose to build biodegradable plastics, chemical precursors, or microbial protein, showing its growing footprint in environmental innovation.
Research & Development
R&D labs keep finding new uses and properties in glucose. Analytical chemists refine sensors for blood glucose, using enzymatic and fluorometric detection. Researchers examine how glucose metabolism shifts in cancer cells, chasing weaknesses to design new therapies. Synthetic biologists harness engineered yeast strains, coaxing them to turn glucose into rare pharmaceuticals, vitamin precursors, and high-value flavors. Nutritionists unravel its changing role in modern diets, linking spikes and dips with cognitive performance or metabolic syndrome. Ongoing work explores low-glycemic glucose analogues for diabetic diets, and residue-free methods to purify glucose from agricultural byproducts, aiming to balance affordability and environmental burden.
Toxicity Research
Though fundamentally a natural metabolite, the discussion around glucose’s toxicity focuses on context and dose. Acute exposure at pharmaceutical doses remains safe for most, aside from rare hypersensitivity or metabolic errors such as glucose-6-phosphate dehydrogenase deficiency. Chronic overconsumption, especially in the context of processed foods and sedentary habits, tracks closely with rising rates of type 2 diabetes, metabolic syndrome, and non-alcoholic fatty liver disease. Controlled studies show that excess glucose leads to surges in insulin, hepatic fat accumulation, and in rodents, even promotes aging pathways through glycation. Toxicologists look at the question from multiple angles—cell culture, animal models, and epidemiological studies—all signaling that moderation, along with fiber and micronutrients, offer the safest approach. Updating public health guidelines and investing in better food labeling could ease population-level risks.
Future Prospects
Researchers, companies, and public health leaders continue to adjust how they see glucose in future foods and pharmaceuticals. Labs worldwide chase enzymatic and fermentation innovations to extract or synthesize glucose from agricultural waste, aiming to slash costs and carbon footprints. Smart packaging and cheap home test kits may empower people to track intake and blood levels, reshaping clinical practice and personal nutrition. The growing appetite for sustainable chemicals keeps driving glucose-based biorefining, making everything from fermentable jet fuels to PLA bioplastics. Targeted education and reformulation could trim the link between glucose and metabolic disease, reshaping what the next generation eats and drinks. Whether in a rural health post, a biotech clean room, or an automated farm, glucose remains central—yet flexible enough to support both tradition and the boldest new ideas in science and industry.
Not Just a Sugar: Glucose in Everyday Life
Glucose often gets lumped together with other sugars, but this single molecule keeps life running smoothly for people and plenty of other living things. Our bodies never really get a break from needing it. After eating bread, pasta, fruits, or even carrots, glucose flows into the bloodstream. From there, it fuels every cell and powers us through both ordinary days and the moments that push us to our limits. Without enough, the brain starts to slow, energy slips away, and even simple tasks feel harder.
Every Cell’s “Go” Signal
Think about someone working outside in hot weather. Sweat pours, knees start to wobble, and thinking gets fuzzy. Grab a juice box or a piece of fruit, and a few minutes later, hands grow steadier and the mind clears. This jump in energy—familiar to anyone who has felt their blood sugar plummet—shows how quickly the right amount of glucose can revive the body. Hospitals keep glucose solution close at hand for fast energy boosts, especially in emergencies like hypoglycemia or after major surgery. Glucose ensures the heart keeps beating, muscles keep moving, and wounds can heal.
A Lifeline for People with Diabetes
Diabetes changes the game entirely. I have friends whose lives turned upside down because they had to monitor blood glucose numbers so closely. For them, glucose isn’t just nutrition—it’s a number that could determine whether their day continues as planned or ends with a trip to the ER. Glucose monitoring technology has improved safety and independence over the years. Quick-dissolving glucose tablets and drinks can stop dangerous drops in blood sugar right away. Medical teams in ambulances often start with glucose if they aren’t sure whether someone has fainted due to dangerously low levels.
Glucose in Food Production and Industry
Manufacturers rely on glucose syrup to sweeten and preserve foods. Chewy candies, energy bars, jams, and even sauces gain more than taste from this ingredient. It adds texture and helps retain moisture, extending shelf life. Fast energy comes in the form of sports gels, drinks, and snacks, specially marketed to athletes. These products make use of glucose’s ability to pass quickly from the gut into the bloodstream. In my own kitchen, baking with glucose syrup sometimes saves things from drying out or getting crystally, especially in homemade candies.
Beyond the Plate: Other Surprising Uses
Glucose sneaks into pharmaceuticals as a carrier or stabilizer for certain medications. It helps products dissolve or mix more easily, making them safer to inject or swallow. Medical labs use glucose to help grow bacteria and yeast, which then enable researchers to make antibiotics, vitamins, and useful enzymes. Even outside food and medicine, glucose has a place in fermentation for brewing beer and spirits. Its feedstock kicks off the fermentation process that’s been part of human culture for centuries.
Looking Ahead: Finding Balance
Too much glucose in modern diets plays a big part in the rise in obesity and metabolic disease. While glucose never stops being necessary, portion size and balance matter now more than ever. Education, smart food labeling, and more thoughtful cooking can help people find their own healthy balance. Everyone deserves access to tools and trustworthy information to make those choices for themselves.
Looking at Glucose Through a Diabetic’s Eyes
Sugar calls to us from every corner and aisle, but those who live with diabetes read every label knowing each gram matters. Glucose feels both like a friend and a troublemaker in this world. The body usually takes carbohydrates from bread, fruit, and pasta and turns them into glucose. Cells use this as fuel, so without it, we lose energy, focus, and even the will to power through an afternoon. Still, diabetics juggle a tricky balance: enough glucose to keep going, not so much that their blood sugar skyrockets.
The Real Risk Behind Glucose
Every diabetic’s story is unique. My own mother kept hard candies in her purse for years, ready in case her blood sugar crashed. Those candies are pure glucose. In that moment, for someone whose blood sugar sinks too low, glucose doesn’t just help. It can save lives. Glucose tablets and gels pop up in every health kit for diabetics, and doctors recommend them because insulin or certain medications can drive blood sugar down so far that the brain and heart tremble at the edge of disaster.
Here’s where things get tangled. The very substance that pulls someone out of a crisis stirs up problems when it keeps showing up on the daily menu. Glucose and other types of sugar can spike blood sugar if the body’s insulin can’t manage it. Over time, this pushes up risks for blindness, kidney damage, and nerve pain. The American Diabetes Association points to the blind spots of letting glucose, especially in high amounts, sneak in unchecked. The CDC’s recent data highlights climbing rates of diabetes complications, much of it tracing back to high blood sugar.
The Role of Moderation and Smart Choices
Glucose isn’t bad by itself. The issue climbs in when quantities spill beyond what your medication, exercise, or insulin can handle. As a child of a diabetic, I saw how a middle ground meant learning how to swap white bread for whole grain, skipping the second helping of pasta, and saving sweets for real emergencies. Those moments shape every meal. Each person’s threshold differs: some tolerate more, some less, depending on age, medication use, and exercise habits.
Carb counting isn’t just math. It’s empowerment. People use glucose meters and continuous monitors as their watchdogs, making split-second decisions. Research from the Joslin Diabetes Center shows people who stay within a healthy glucose range avoid hospital trips, give themselves a better shot at a solid future, and skip years of complications.
Smarter Regulations, Real-World Results
Shopping trips change when you understand what spikes you. Home-cooked meals beat takeout for a good reason — you see exactly how much sugar gets in. Doctors now teach skills as much as advice: reading nutrition labels, learning how fiber slows sugar absorption, and tracking meals in an app. Many patients turn to diabetes education classes or online groups, trading real recipes and tips. These community resources break the sense of isolation and offer creativity in problem-solving.
We can’t erase glucose from the world, nor should diabetics fear it. Real progress begins with learning, tracking, and choosing foods that respect the body’s limits. Big food companies also face pressure to lower hidden sugars and offer more real choices. Honest discussions between patients and doctors, support from family, and better labeling bring this power back to the people negotiating their relationship with sugar every single day.
Two Words, Many Meanings
Glucose shows up in just about every discussion on diet, diabetes, and energy. Sugar, on the other hand, feels much broader and gets tossed around in everyday talk: “sugar makes you fat,” “cut back on sugar,” “fruit has too much sugar.” Yet, most people mean the white stuff in a sugar bowl, not realizing that “sugar” refers to a family, not a single thing. That’s where confusion sneaks in.
Defining Glucose and Table Sugar
Straightforward science says glucose is a single molecule—one unit. It fuels every cell, especially the brain. Bread, potatoes, and honey all deliver glucose directly or break down into it during digestion. The word “sugar” covers more ground. Sucrose, better known as table sugar, comes from sugarcane or sugar beets. When you eat it, enzymes split each molecule in half: one part glucose, one part fructose.
So, the body sees “sugar” as a package deal—sometimes as single units like glucose (in fruit and starchy foods), sometimes as pairs like sucrose, lactose (milk sugar), and maltose (grain sugar). As soon as these hit your gut, everything gets sorted into glucose, fructose, or galactose before heading toward your bloodstream.
Why the Distinction Matters
Many years working with people living with diabetes showed me how knowing the difference between glucose and other sugars trumps just counting “sugars” on a label. Glucose pushes blood levels up quickly because it enters straight into the blood during digestion. Sucrose takes a pit stop; it splits into glucose and fructose before both hit the system.
The pancreas responds most aggressively to glucose, triggering insulin—a hormone that shoves glucose into cells for energy or storage. Fructose fades into the background, handled mostly by the liver. Too much fructose may burden the liver, shifting some into fat, but doesn’t spike blood sugar the same way.
Many health problems—type 2 diabetes, metabolic syndrome, fatty liver disease—link to diets heavy in added sugars and refined starches. Foods high in glucose or quickly breaking down into it drive blood sugar swings and cravings. Swap these for whole grains and fiber-rich produce, and the body handles sugar intake better. Eating in this way means the digestive process slows down, so glucose reaches the bloodstream gradually, keeping energy and mood steady.
Spotting Glucose and Sugar on Labels
Product labels rarely make things simple. “Sugars” on packaging bundles glucose, fructose, and several others. Corn syrup and honey sound worlds apart, but both offer lots of glucose.
One smart move—scan labels for the grams of “added sugars.” If you see ingredients like high-fructose corn syrup, maltose, or even glucose syrup, you’re getting processed sources. Fruit and milk list “sugar” too, but those come as part of a package that offers fiber or protein, making the sugar hit much milder.
Looking Forward: Small Steps Make a Difference
Most families benefit just by replacing sodas and highly processed snacks with homemade meals and whole foods. Cooking at home cuts down on “hidden” sugars and lets you see exactly what goes on your plate. Reading labels helps, but getting used to the taste of less sweet things changes habits for good.
Understanding the real difference between glucose and sugar arms you with knowledge. That makes it easier to push back against confusing food fads—and take charge of health one bite at a time.
Why Glucose Gets Attention
Glucose shows up everywhere. Many people know it as the sugar doctors measure in blood tests. Athletes down glucose gels for quick energy. People with diabetes use glucose tabs to avoid dangerous blood sugar crashes. It seems pretty harmless at first glance—a simple sugar, something bodies rely on for fuel. Over the years, though, stories keep surfacing about unexpected downsides. It’s not an ingredient to take casually, especially outside critical situations.
Common Side Effects and Reactions
Most folks who eat or drink glucose in moderate amounts notice nothing ugly. Still, after spending years listening to patients and scouring research, I keep seeing the same patterns. People can get:
- Nausea or stomach aches. Stomach discomfort hits after a high dose, especially with syrups or very sweet drinks.
- Blood sugar spikes. A sugar rush gets thrown around as a phrase, but glucose shoots blood levels higher, and sometimes too fast. That matters for folks with insulin resistance, prediabetes, or diabetes—sharp peaks feel awful and drag energy levels down after the high.
- Dehydration. Glucose pulls water into the gut and out of the blood, so after big doses, some people feel thirstier or pee more often.
- Mood swings or fogginess. When blood sugar shoots up, focus drops for some. After the spike, fatigue and crankiness follow. I’ve seen parents call out the “meltdown” after a birthday party sugar binge—the pattern rings true with added glucose, not just candies.
When Glucose Turns Risky
Glucose offers a fast fix for someone with low blood sugar. Beyond emergencies, taking it without need adds risks. Long-term excess increases the chance for Type 2 diabetes, heart trouble, nerve damage, and vision loss. The American Diabetes Association points to the role of high blood sugar in damaging blood vessels. The story is clear—using glucose too freely can drag health downhill.
Some people are more vulnerable than others. A family member with digestive trouble discovered her gut can’t handle rapid shifts from high glucose. She started fainting and developed headaches. She was told by her doctor to stop the glucose chews and go back to small, balanced snacks instead.
Making Safer Choices
No food or supplement comes without a tradeoff. The question isn’t whether glucose is “good” or “bad,” but who should take it, and in what amounts. Health professionals stress the importance of measuring blood sugar levels before grabbing glucose as a remedy. It makes sense to reach for fruit or a starchy food like bread most of the time instead. Those choices don’t catapult blood sugar as quickly, and come with vitamins, fiber, and less risk of side effects.
Many athletes I’ve spoken with stick to lower-glycemic options in training and reserve glucose gels for only the longest workouts. People with diabetes learn quickly to check blood sugar before taking any supplement; guessing leads to wild rides nobody enjoys.
Real solutions lie in awareness and moderation. Taking glucose for a real medical reason is safe—just check label doses and don’t use it as an excuse to eat more sugar everywhere else. Doctors and nutritionists can help sort through confusing advice and create safer routines. Glucose isn’t the villain, but overdoing it usually leads to trouble down the road.
How Glucose Fuels Your Workout
Take a look in any sports drink bottle, and you’ll see glucose front and center in the ingredients. It matters because glucose acts as your body's most direct fuel, especially when sweat pours and legs keep turning. I’ve seen plenty of runners try to “train low,” skipping carbs to force their bodies to use fat. Most of them hit the wall hard. Science backs up what those runners felt—the fastest way the body produces usable energy, especially in intense workouts, is by tapping into its glucose stores.
Muscles pull glucose from the blood. Your liver and muscles store extra as glycogen—essentially, compact energy packets—so you can call on them fast. Glycogen stores are limited. That’s the catch that beginners often overlook. Going out hard on a long run or high-intensity interval session without enough glucose leaves you dragging by the halfway point.
Why Glucose Really Matters Under Stress
Exercise causes muscles to contract and energy demand heats up. Glucose turns into ATP—the body’s currency for movement—through glycolysis. This pathway pumps out energy much quicker than burning fats. Think about lifting a heavy barbell or sprinting after a bus. Slow-releasing energy can’t keep up. Bodies built for performance depend on fast glucose-driven energy.
After working with high school athletes during track season, I saw that those who took in carbohydrates before and after workouts bounced back faster. Their tiredness faded quicker, soreness didn’t linger, and their focus sharpened the next day. Studies agree: giving the body carbohydrates before, during, and after exercise keeps blood glucose levels stable and improves endurance.
Downsides of Running Dry on Glucose
Skipping carbs or not refueling during endurance events means running low on glucose. Symptoms creep in—a fuzzy brain, heavy legs, chills. That “bonk” feeling comes from empty glucose tanks. Glycogen depletion pushes the body to burn stored fat, but this method works far slower and comes with performance trade-offs. Fat metabolism can’t keep pace during high effort. There’s a reason marathoners and cyclists crave gels and chewy blocks.
Low glucose doesn’t just hurt performance; constant depletion strains the immune system and recovery. Over time, intense training without enough refueling raises stress hormone levels, leading to burnout or injury. Every endurance coach stresses post-workout nutrition for good reason.
How to Optimize Glucose Use in Exercise
Most can improve energy by eating balanced meals with enough complex carbohydrates. Bananas, rice, potatoes, oats—these top up glycogen before a hard effort. During longer efforts over 60 minutes, quick-digesting carbohydrates like sports drinks or fruit work best for topping up. I’ve tried going without mid-run snacks, and my pace always slips. Refueling isn’t just about avoiding a crash—it also sharpens focus, coordination, and enjoyment.
Experience and studies tell the same story: giving the body enough carbohydrates, especially before strenuous or long exercise, lets it run smoother and recover faster. The more intense or longer the effort, the more important glucose becomes. The best routine tailors intake to activity type, individual needs, and personal comfort. Always remember, food is fuel.

| Properties | |
| Acidity (pKa) | 12.46 |

